Fighting with your insurance company over a treatment you need? Don’t let insurance red tape delay the care you deserve. A Letter of Medical Necessity Template (LMN) can be your key to getting the treatment you need covered.
What is a Letter of Medical Necessity (LMN)?
The Basics: It’s a formal letter written by your doctor to your insurance company. The letter explains exactly why you need a specific treatment, medication, piece of medical equipment, or service.
When You Might Need an LMN
Here’s a situations where a (LMN) is commonly needed, with some additional examples:
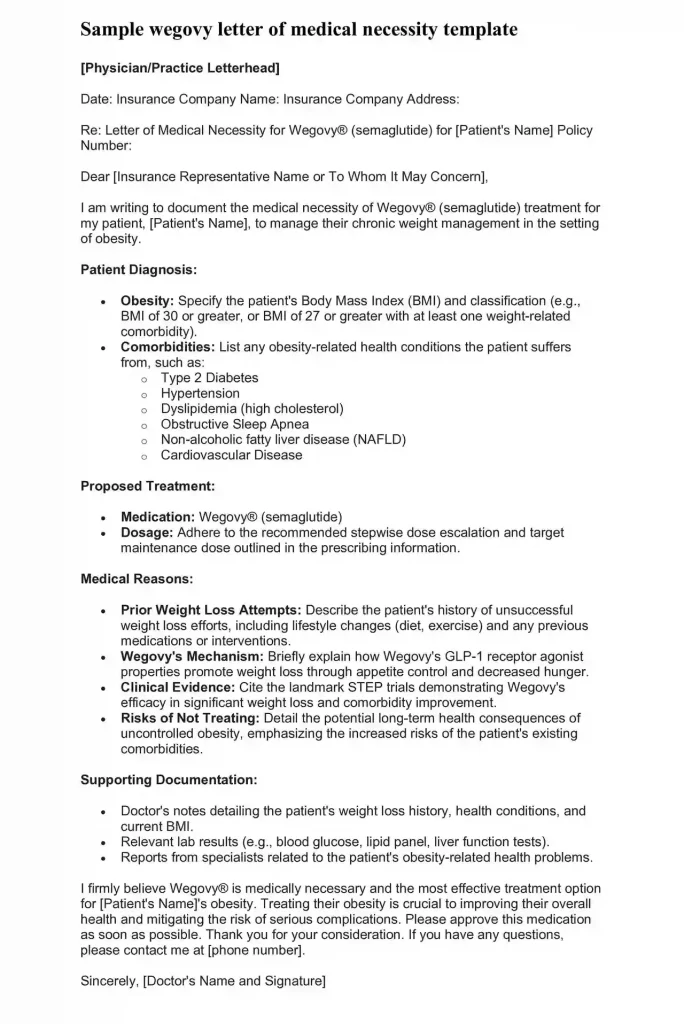
Expensive Medications
Insurance companies often want extra proof before approving pricey medications, especially:
- Brand-name drugs when a generic version exists
- Newer medications without a long track record
- Drugs not typically used for your specific condition
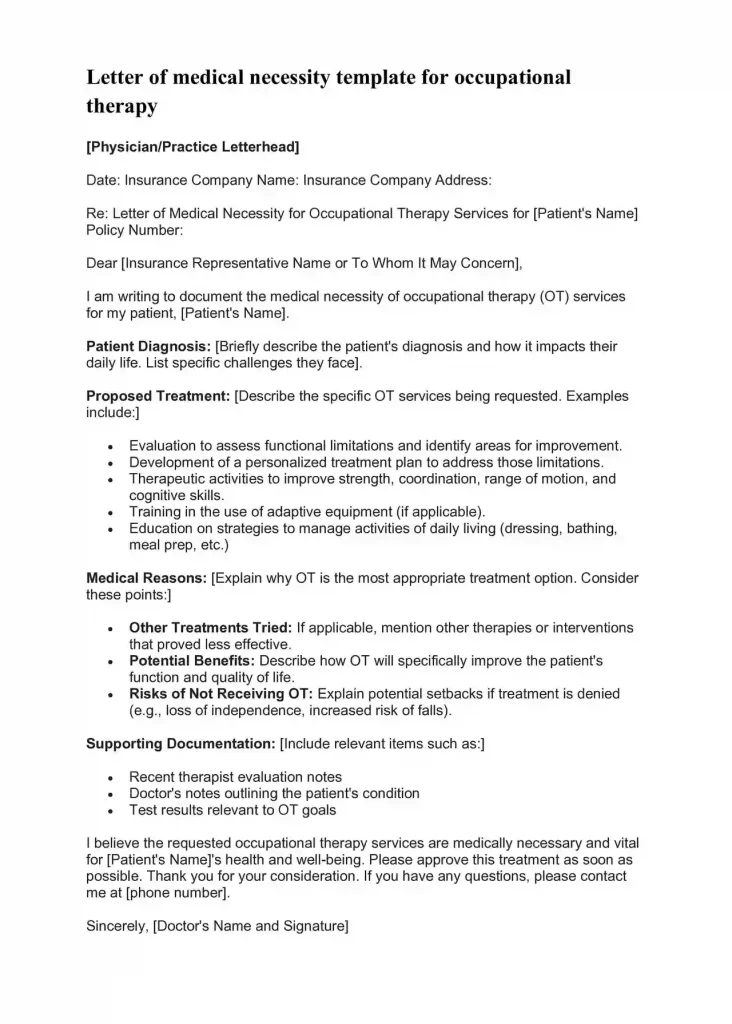
Specialized Therapies
If your doctor recommends ongoing therapy, you might need an LMN, especially for:
- Physical therapy after an injury or surgery
- Occupational therapy to help with daily life skills
- Speech therapy for communication difficulties
- Mental health therapy (counseling or specialized treatments)
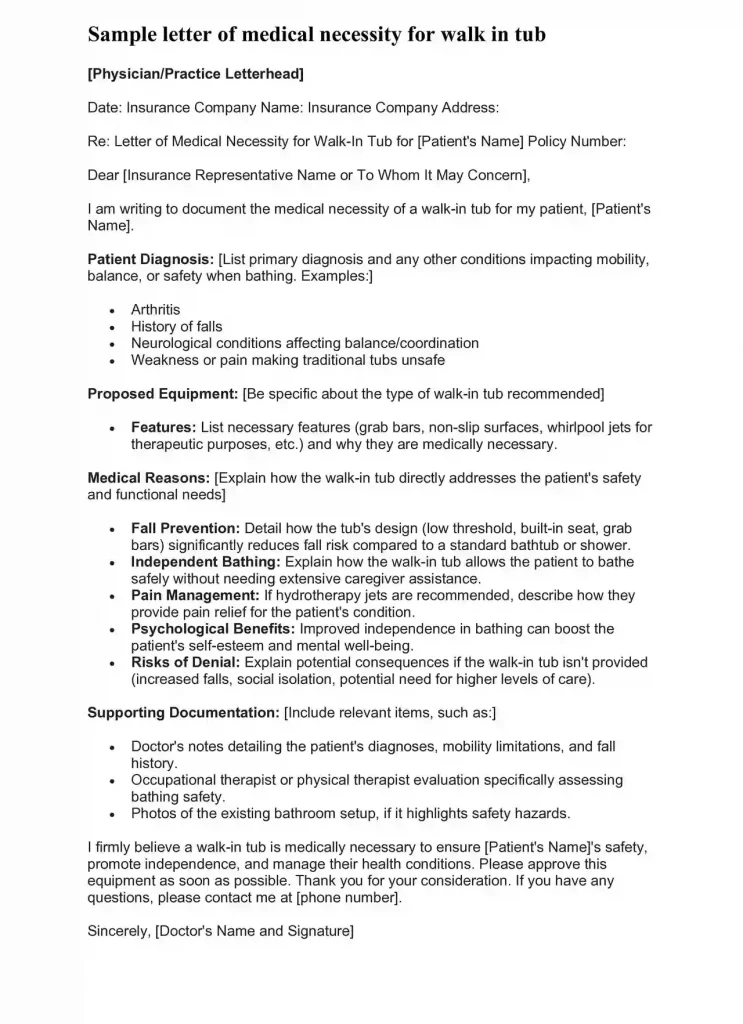
Medical Equipment
This category is broad! LMNs are common if you need:
- Durable Medical Equipment (DME): This includes things like wheelchairs, walkers, hospital beds, oxygen equipment, etc.).
- Prosthetics or orthotics: Custom-made devices or braces
- Specialized home modifications: Like wheelchair ramps or bathroom grab bars
Surgeries or Complex Procedures
LMNs may be required for:
- Surgeries, especially elective or less common ones
- Inpatient hospital stays for treatment
- Imaging tests: Like advanced scans (MRIs, CT scans) or genetic testing
Important Notes
- Every Insurance is Different: Some insurers require LMNs more often than others. The best way to know is to check your policy or call your insurance company.
- Doctor’s Recommendation is Key: Ultimately, your doctor will tell you if they think an LMN is necessary to increase your chances of getting the treatment covered.
How to Write a Letter of Medical Necessity and Get Your Treatment Approved
Here’s a breakdown of the tips:
Understand Why You Need an LMN
- Focus on the Basics: Begin with a simple definition and explain when an LMN would be needed.
- Example: “Sometimes your insurance won’t pay for certain treatments or equipment unless your doctor writes a special letter. This is called a Letter of Medical Necessity (LMN).”
Gather Your Information
- Keep it Simple: List the most important items a patient should gather rather than overwhelming them with a complex list.
- Use Plain Language: Replace words like “relevant” with simpler terms like “important”.
Talk to Your Doctor
- Clear Actions: Instead of “initiate the conversation”, use action-oriented terms like, “Ask your doctor…”
- Add Patient Perspective: Emphasize that a patient can bring valuable information to this conversation.
Why are LMNs Important?
Insurance companies are in the business of managing costs. An LMN from your doctor provides them with the justification to approve a treatment. It demonstrates that the recommended treatment is:
- Showing “Medical Necessity”: Insurance companies don’t pay for just anything. Your doctor’s LMN shows that the treatment is really needed to manage your condition, not just something extra.
- Avoiding Unexpected Costs: Without an LMN, your insurance might not pay for your treatment. This could leave you with a big bill. A good LMN helps you get approval beforehand. This gives you peace of mind.
- Preventing Delays in Care: When coverage is a problem, it can be frustrating to wait for the treatment you need. An LMN helps speed up the approval process so you get care faster.
- Fairness and Access: LMNs help make things fairer. They make sure decisions about your health are based on your doctor’s advice, not just your insurance company trying to save money.
- Empowering Patients: Your doctor writes the LMN, but understanding them helps you stay informed about your health journey. This lets you speak up for yourself and get the best care.
Without a persuasive LMN, you might be left with hefty medical bills or have to delay important care.
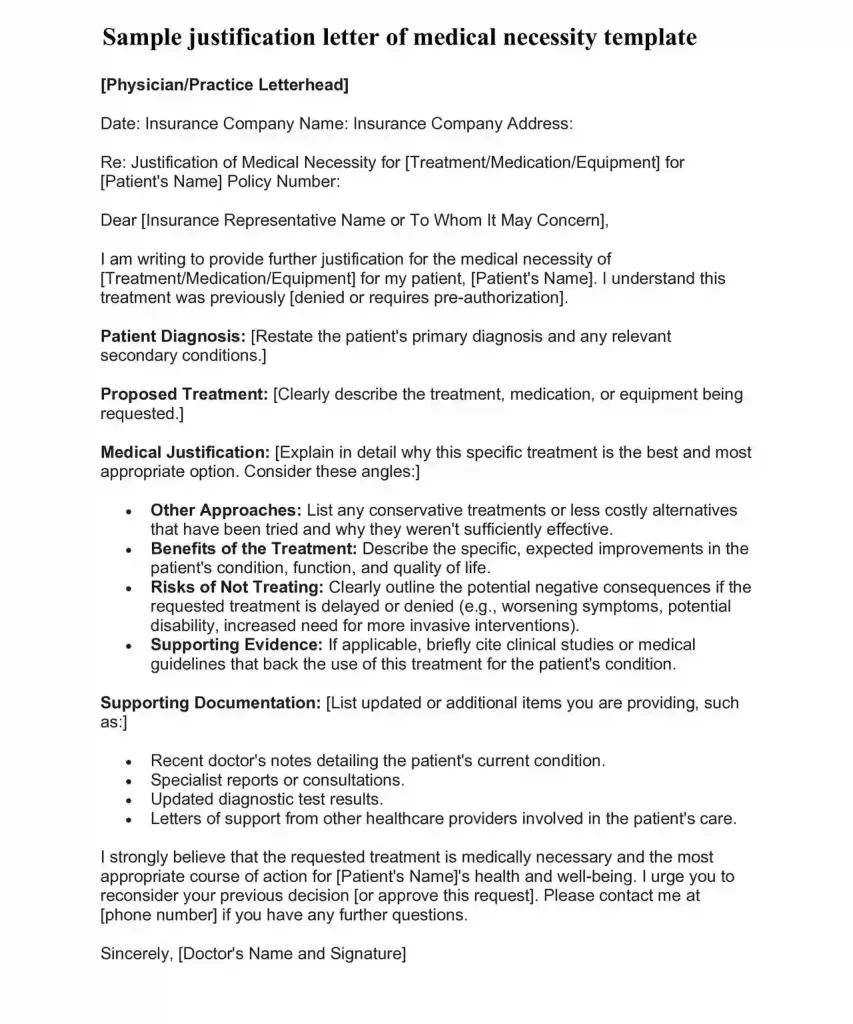
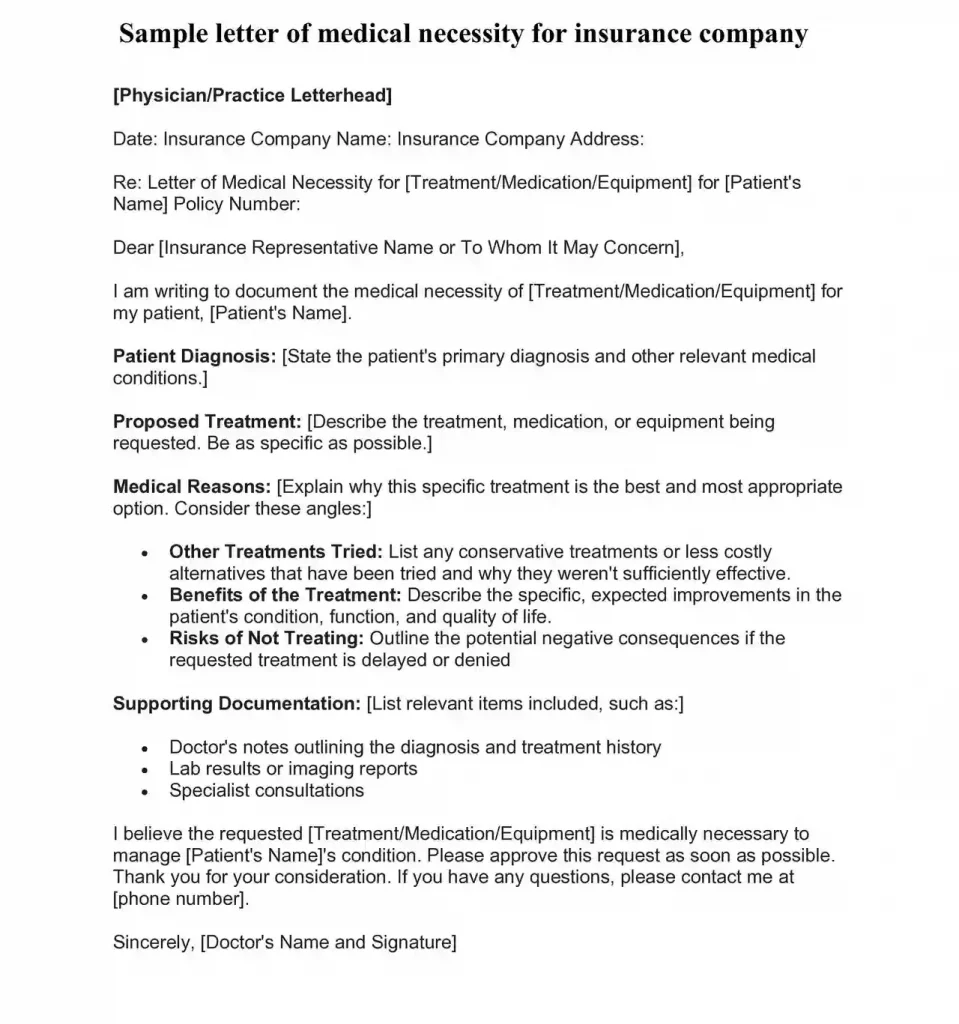
Key Components of an Effective LMN
Your doctor handles the bulk of writing an LMN, but understanding the pieces helps you be a better partner in the process. Here’s what a strong LMN includes and why it’s important:
1. Your Information: Name, date of birth, and insurance details.
Why it matters: This seems basic, but it lets the insurance company be 100% sure they’re looking at the right person’s file and policy.
2. Diagnosis: The name of the specific health problem you have.
Why it matters: Insurance companies have rules about which treatments are approved for different conditions. Being specific and accurate is crucial!
3. Proposed Treatment: A clear description of the treatment, medicine, or equipment your doctor suggests.
Why it matters: The insurance company needs to understand exactly what they’re being asked to pay for. Is it a specific physical therapy? A 6-week medication trial? The more detailed, the better.
4. Medical Reasons: Your doctor’s explanation of why this specific treatment is the best choice for you.
Why it matters: This is the heart of the LMN! Insurance companies want proof this isn’t just a ‘nice to have’ thing. Your doctor might explain:
- Other options were already tried but didn’t work.
- The risks of NOT doing this treatment are serious.
- This is the standard of care for your condition, backed up by research.
5. Supporting Documentation: Test results, notes from other doctors, etc.
Why it matters: Think of this like “showing your work” on a math test. It’s not just about your doctor saying you need something – it’s about proving why.
Extra Tip: Ask your doctor for a copy of the LMN they submit. This helps you stay informed and double-check that all the information is accurate.
How to Get Your Doctor to Write an LMN
Getting your doctor on board is key to a strong LMN. Here’s how to make this process smoother:
Be prepared
- Medical Records: Have copies of tests, doctor’s notes, or anything related to your condition ready for your appointment.
- Insurance Rules: Try to understand the basics of your insurance policy. Do they usually need LMNs for the kind of treatment you need? Check your insurance company’s website or call them with questions.
- What’s Needed: Do you need medication, equipment, a certain kind of therapy? Be clear on exactly what you’re asking for.
Start the Talk
- Be Direct: Don’t be afraid to say, “My insurance might need a Letter of Medical Necessity for this treatment. Can you help me with that?”
- Explain Why: Let your doctor know if you’re worried about the cost being denied or your treatment being delayed.
- Show You’re Prepared: Having your records organized and understanding your insurance shows you take this seriously.
Teamwork
- Offer to Help: Ask your doctor, “What information would make the strongest letter? Can I help find anything?”
- Be Understanding: Doctors are busy! If they ask you to provide some information first, do it promptly and accurately.
- Follow Up: If you haven’t heard about the LMN after a reasonable time, a polite call or email reminder to your doctor’s office is okay.
Extra Tip: Sometimes the doctor’s office staff actually handles the nuts and bolts of the LMN. Building a positive relationship with them can be helpful, too!
What to Do After Your LMN is Submitted
Waiting for a decision on your LMN can be nerve-wracking. Here’s what to expect and how to handle different outcomes:
The Waiting Game
- Patience is Key: Each insurance company has different timeframes for decisions. Your doctor’s office might be able to tell you what to expect.
- Track It: Write down the date you sent the LMN and any reference numbers you’re given.
- Don’t Panic: Sometimes approvals just take time, so try not to worry too much during this phase.
If Your LMN is Approved
- Celebrate! This means your insurance should cover the treatment your doctor recommended.
- Double-Check: Contact your insurance to confirm the details – are there any costs you’ll be responsible for?
- Move Forward: You can now schedule your treatment or get the equipment or medication you need!
If Your LMN is Denied
- Don’t Give Up: Insurance denials are common, but they’re not always the final word.
- Get Specifics: Call your insurance company and ask for the exact reasons they denied your LMN. Write everything down!
- Talk to Your Doctor: Share the denial reasons with your doctor. They can help you decide if it makes sense to appeal.
- The Appeal Process: Appealing a denial means writing a letter explaining why you disagree and asking your insurance to reconsider. Your doctor may need to add more information to support your case.
- Get Help: This process can be confusing. Many patient advocacy groups specialize in helping people with insurance appeals. Search online or ask your doctor’s office for recommendations.
Printable Free Letter of Medical Necessity Template [Word &PDF]
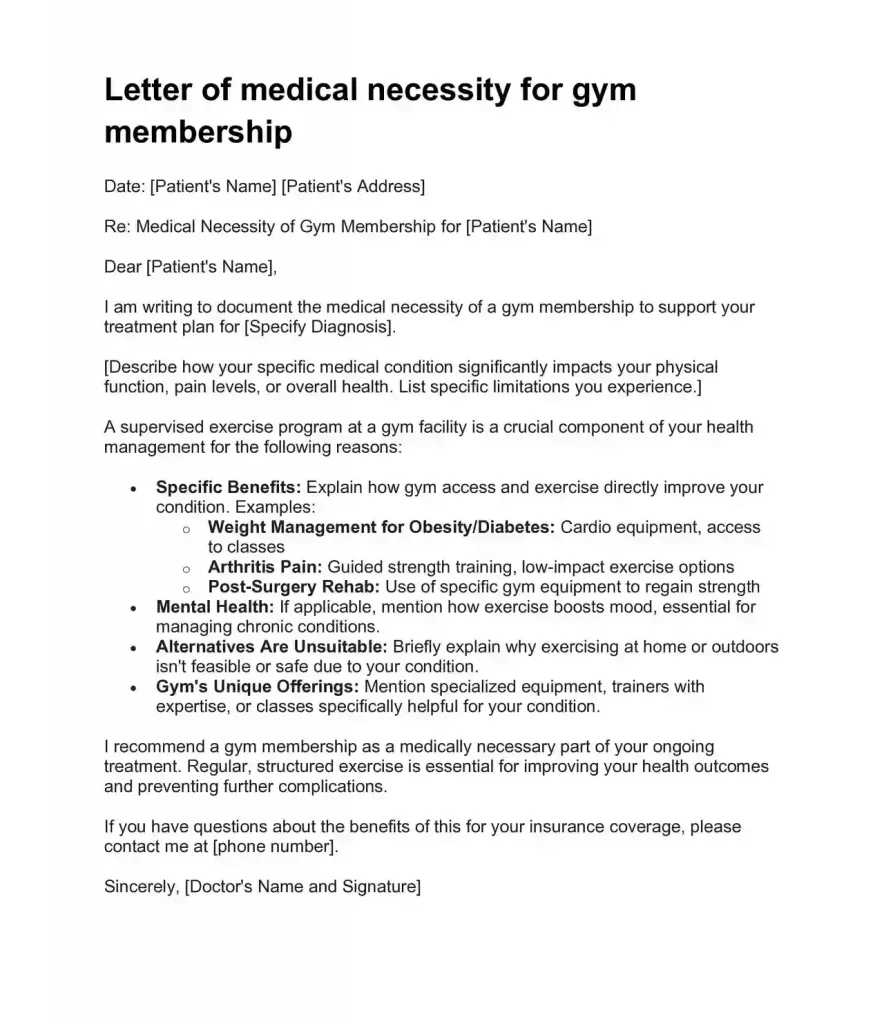
letter of medical necessity for gym membership
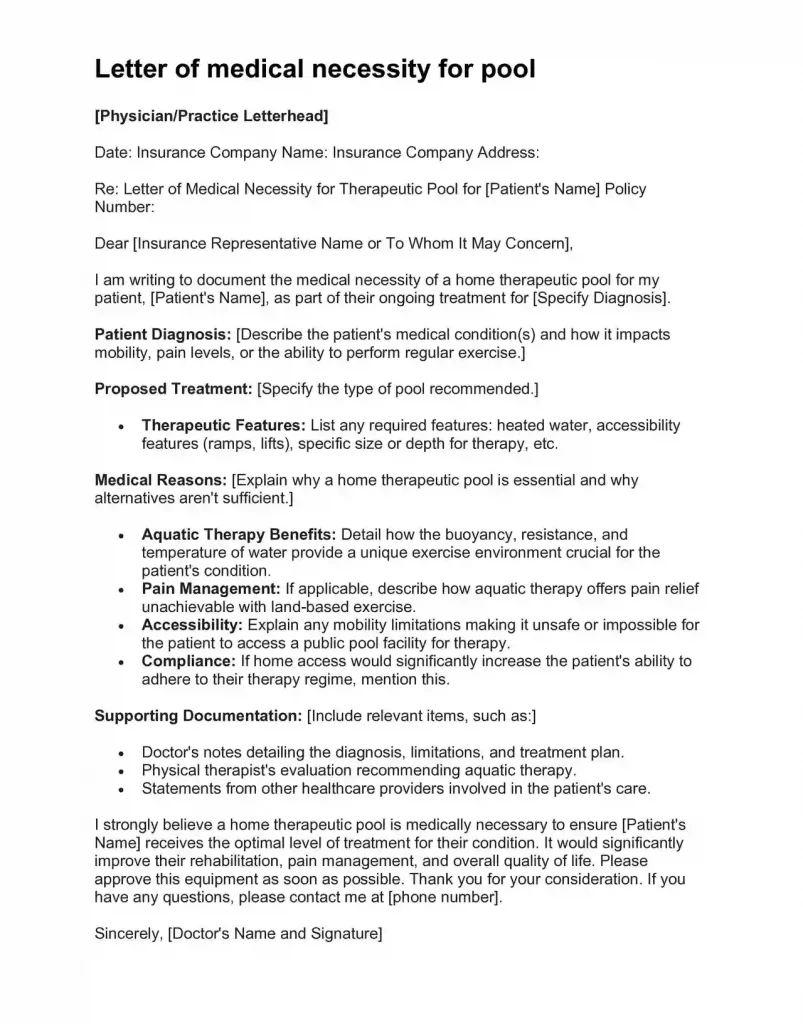
letter of medical necessity for pool
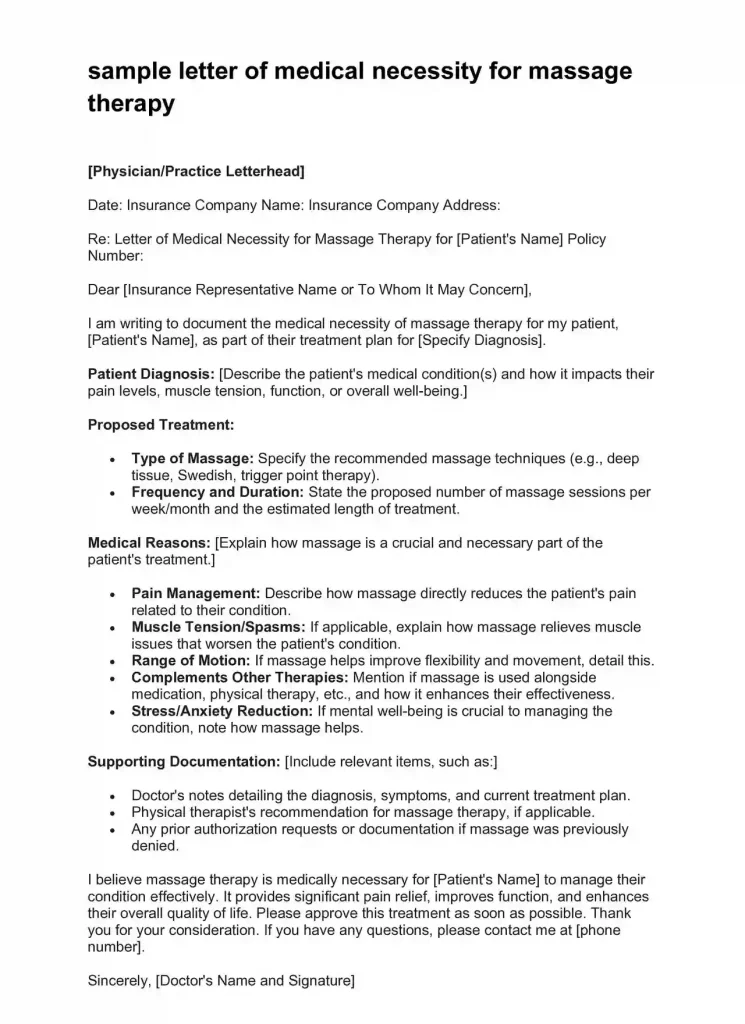
letter of medical necessity template for massage therapy
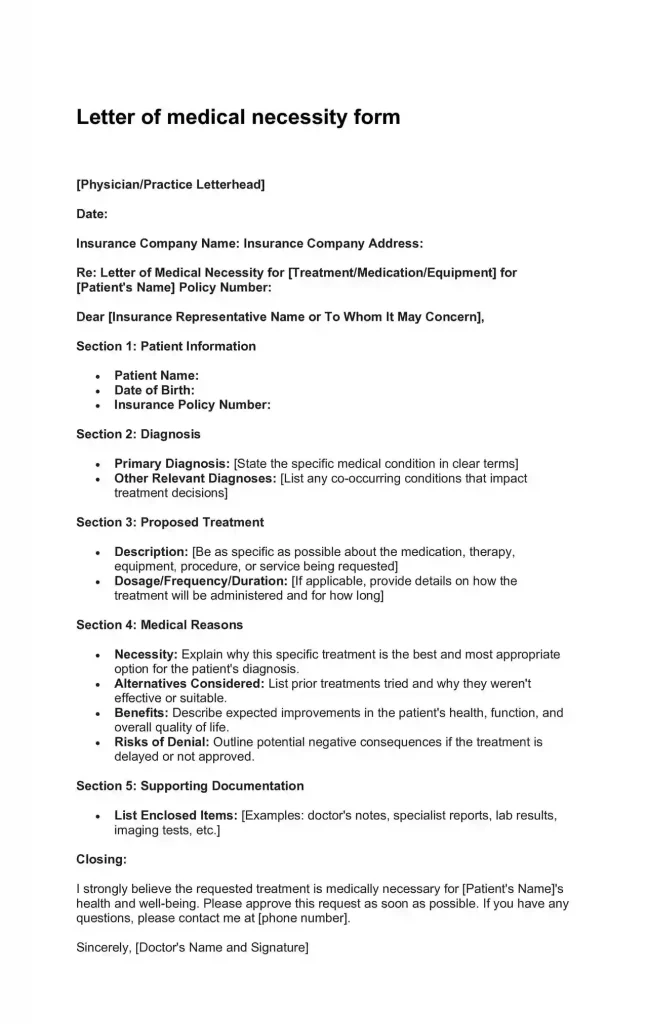
letter of medical necessity form
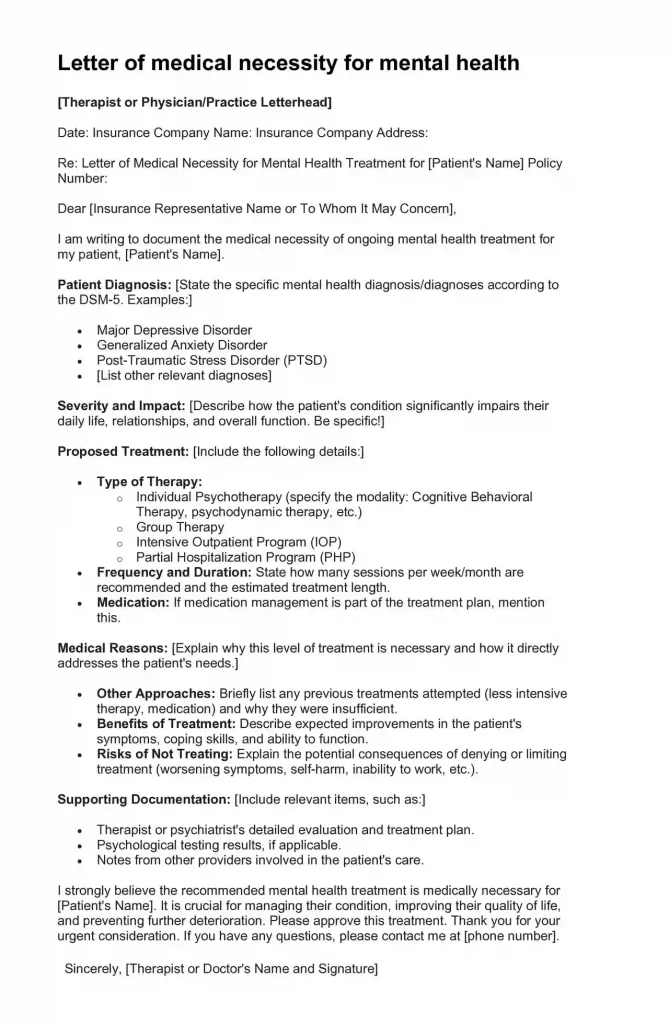
Letter of medical necessity for mental health
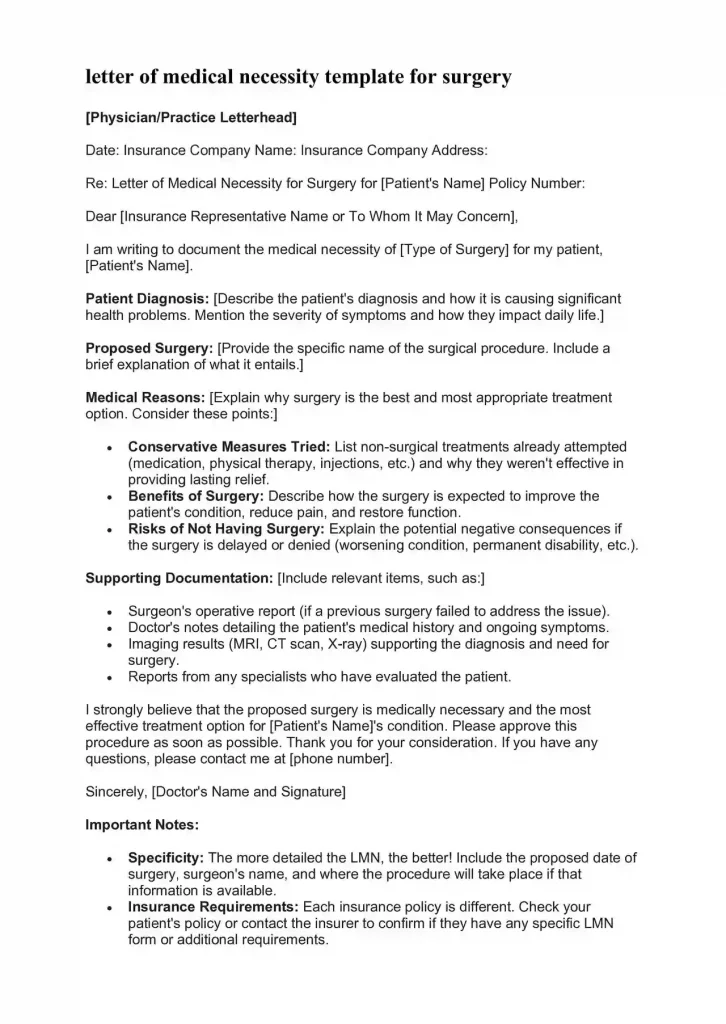
letter of medical necessity template for surgery
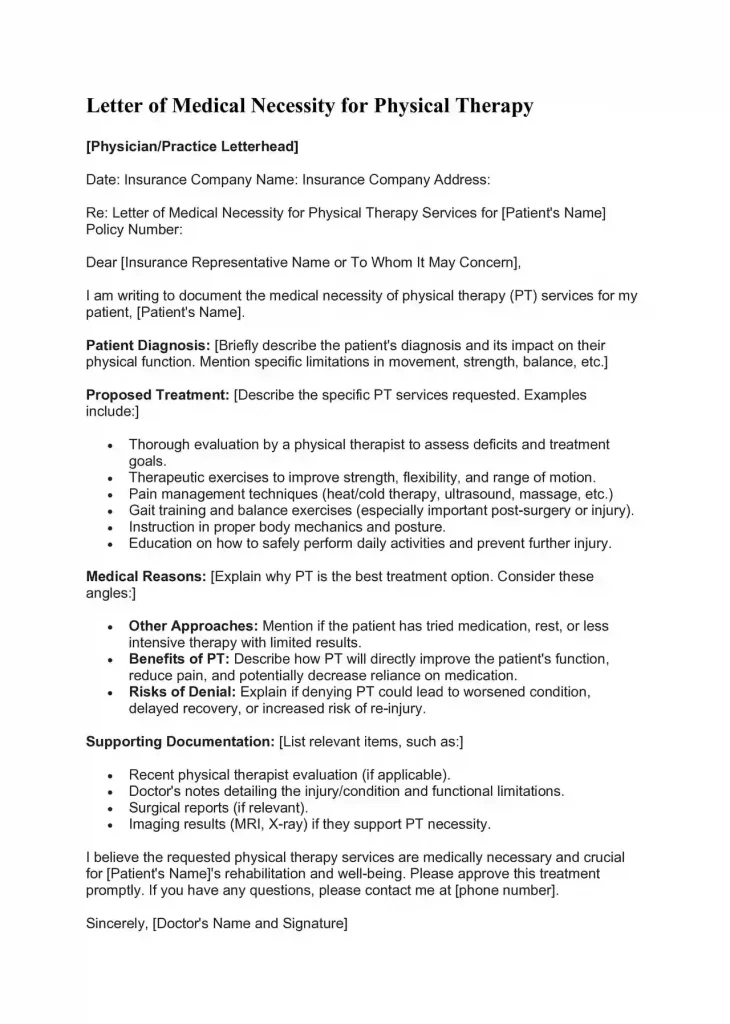
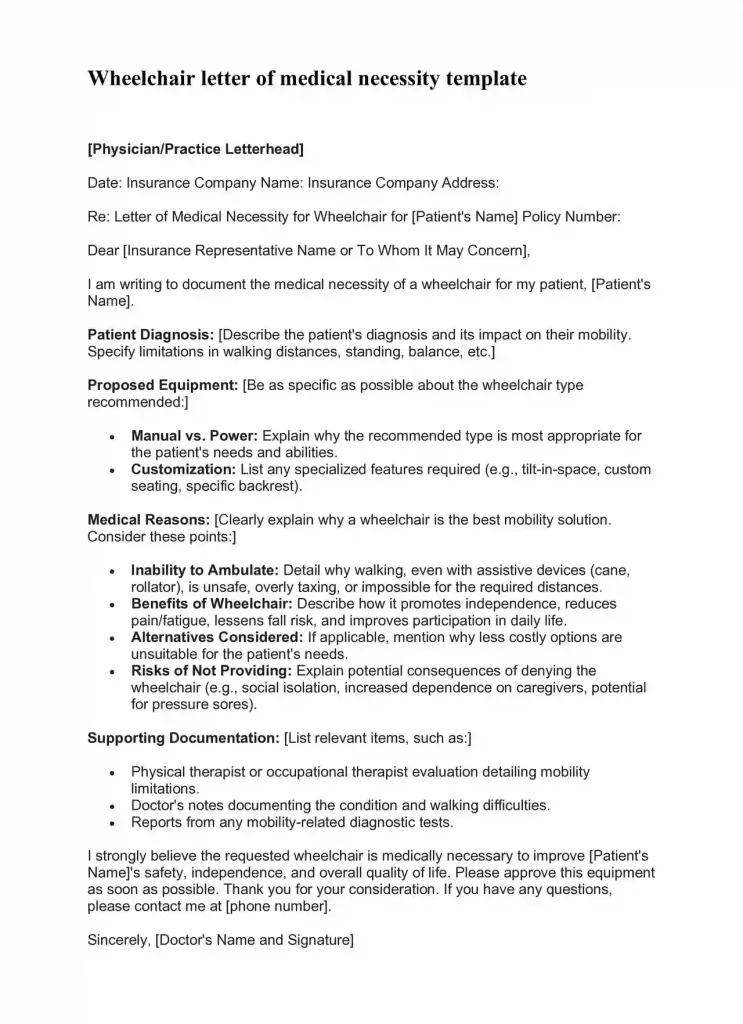
wheelchair letter of medical necessity template
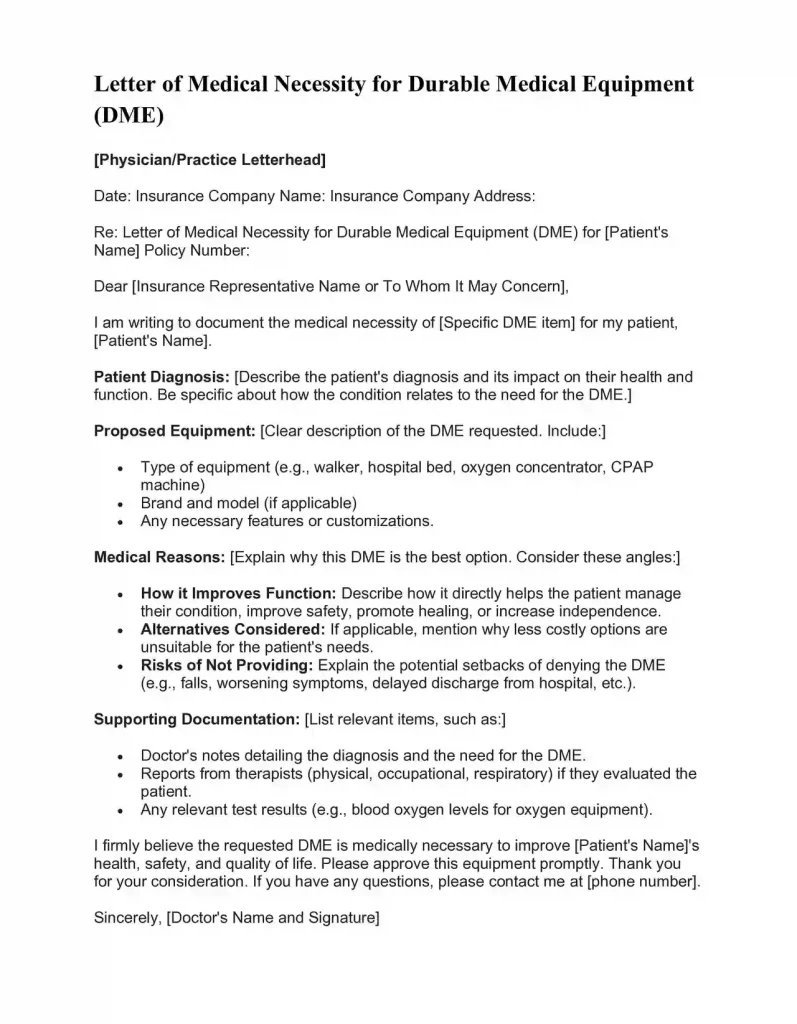
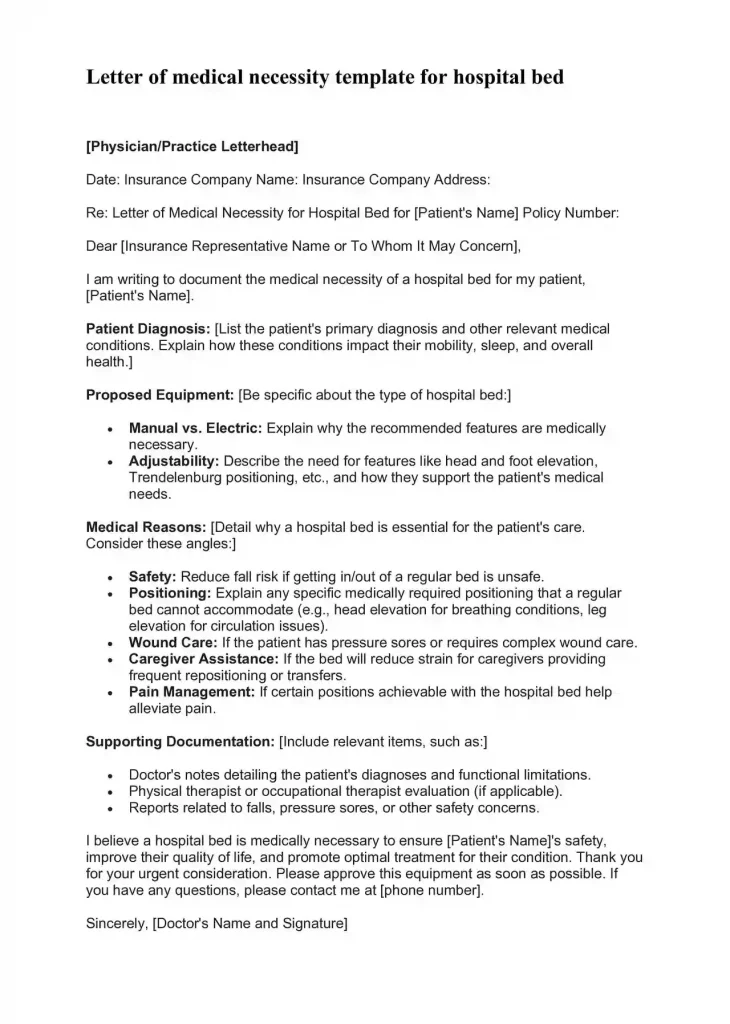
letter of medical necessity template for dme
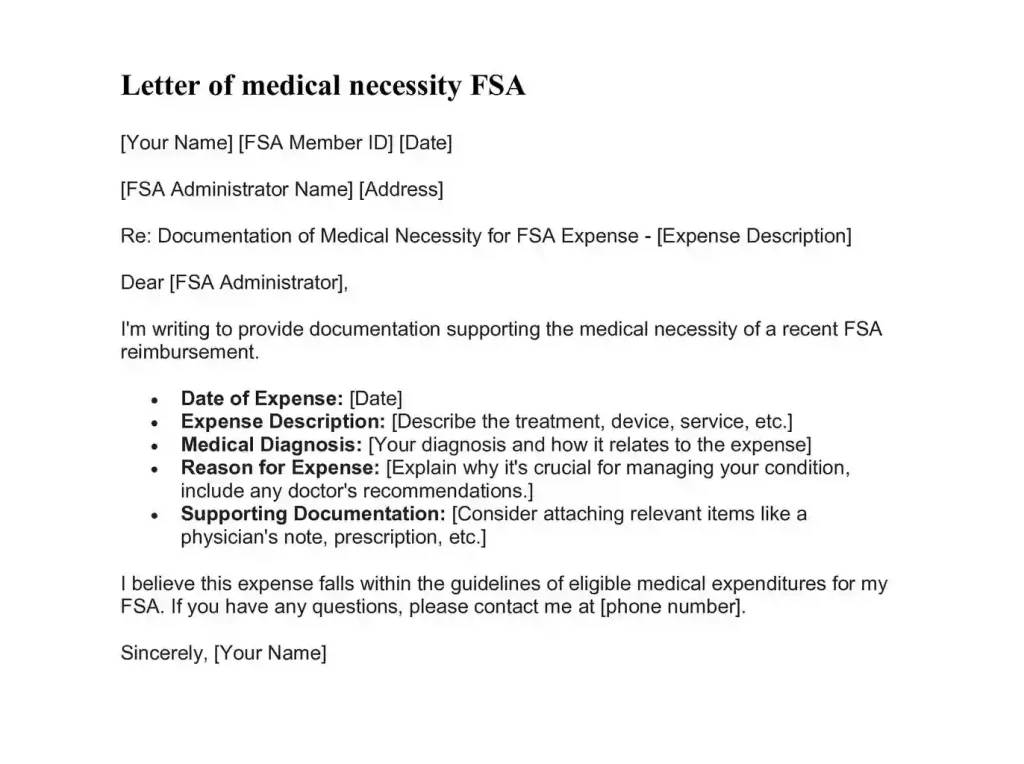
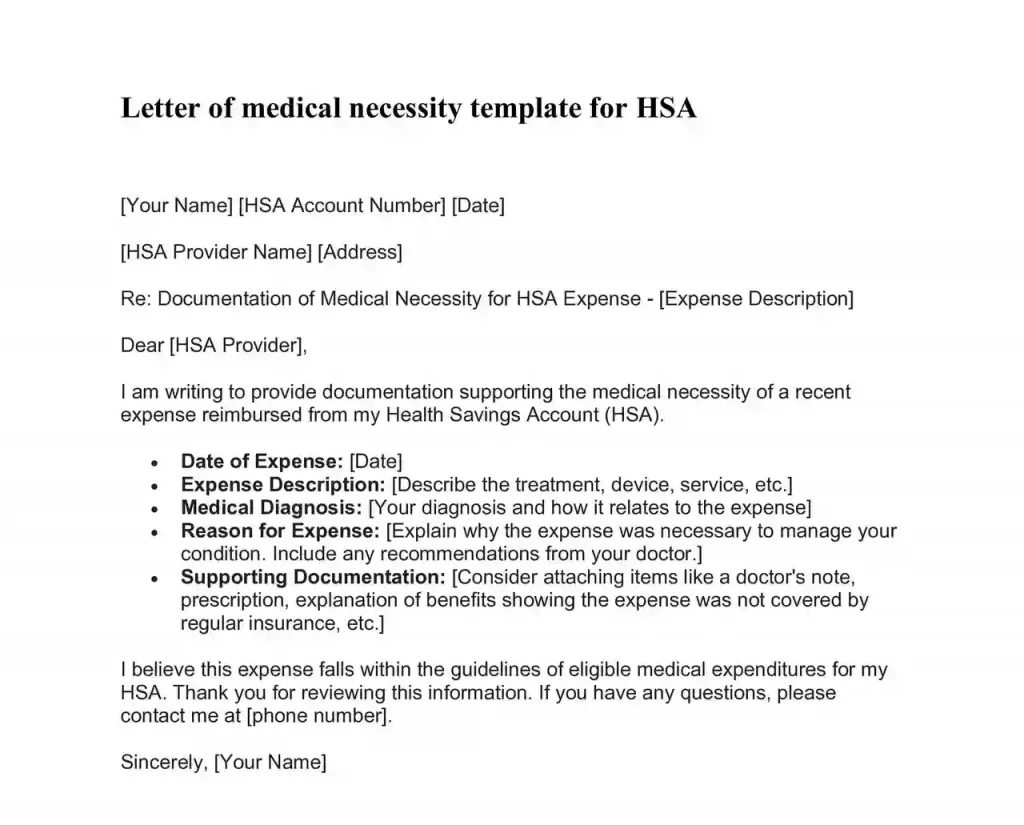
letter of medical necessity template for hsa
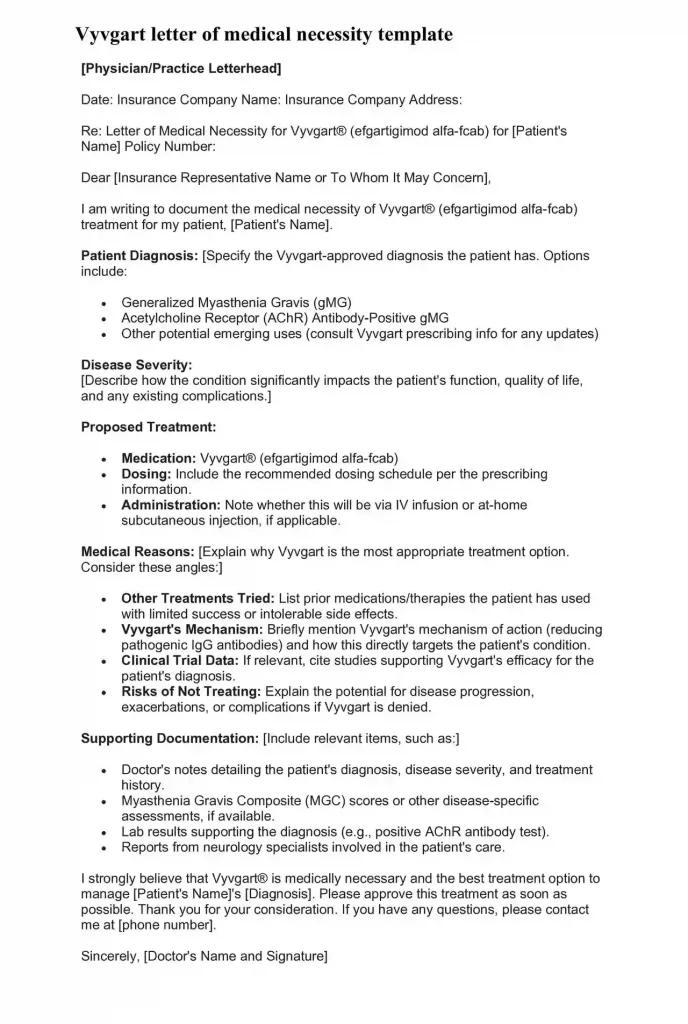
vyvgart letter of medical necessity template
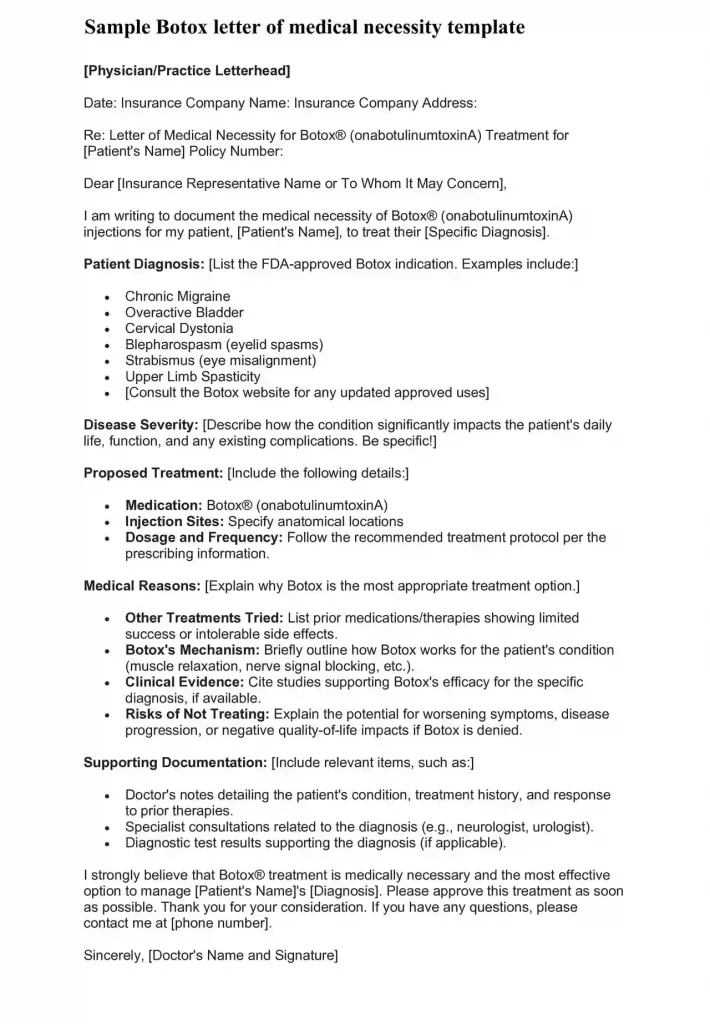
Botox letter of medical necessity template
Conclusion
Letters of Medical Necessity may seem daunting, but understanding them puts you in a stronger position. Be proactive, communicate clearly with your doctor, and know that advocating for the care you deserve is absolutely essential.
FAQs About Letters of Medical Necessity
Can I write my own LMN?
No. While you can provide information to support your case, only your doctor has the medical expertise to write an effective and persuasive LMN.
What if my insurance denies coverage even with an LMN?
Don’t give up! You have the right to appeal the denial. Your doctor can help strengthen the appeal, and many patient advocacy groups offer assistance with this process.
How long does it take for insurance to make a decision after receiving an LMN?
This varies greatly by insurance company. Your doctor’s office may be able to give you an estimate, or you can call your insurer for their typical timeframe.
Will an LMN guarantee my treatment is covered?
Unfortunately, no. However, it significantly increases your chances of approval compared to not having one.
Can I get an LMN for a treatment I already started?
Sometimes, but it’s much riskier. Insurance companies prefer to approve treatments beforehand. If you’re already in treatment, speak to your doctor right away about an LMN.
Who should I contact if I have questions about my LMN?
Start with your doctor’s office. They may have staff who handle LMN submissions and insurance questions.
Does Medicare require LMNs?
Yes, Medicare often requires LMNs, especially for durable medical equipment, specialized therapies, and certain procedures.
What resources are available if I need help with an LMN or an insurance appeal?
Many patient advocacy groups specialize in this area! Search online for organizations related to your specific condition, or ask your doctor’s office for recommendations.

The content creator team at calipsotree.com is dedicated to making topics accessible to everyone, with over 9 years of experience in writing and breaking down complex concepts into easy-to-understand articles that answer readers’ financial questions.